When it comes to the health plan member experience 2022 will be the last year that CMS will give today’s payer a grace period due to the COVID-19 pandemic, where if a measure-level star rating was lower in the current year, the plan is able to revert back to the higher rating from the prior year. If there was ever a time when plans need to prioritize member experience measures, it is now.
As an industry we are seeing the quality of the consumer journey increasingly having a more substantial (and more negative) impact on star ratings and corresponding Quality Bonus Payments (QBP). Then there is the issue of member churn, with more individuals than ever before choosing to leave their plan. To understand the magnitude of the impact, a plan that has 100,000 members with a capitation payment of $840 per member per month and a 13% churn rate will lose $131M in reimbursement. Reducing plan churn by 5% (to a churn rate of 8%) will increase revenue by $50M. This is why member experience is expected to be the primary plan performance driver for Medicare Advantage in the year ahead.
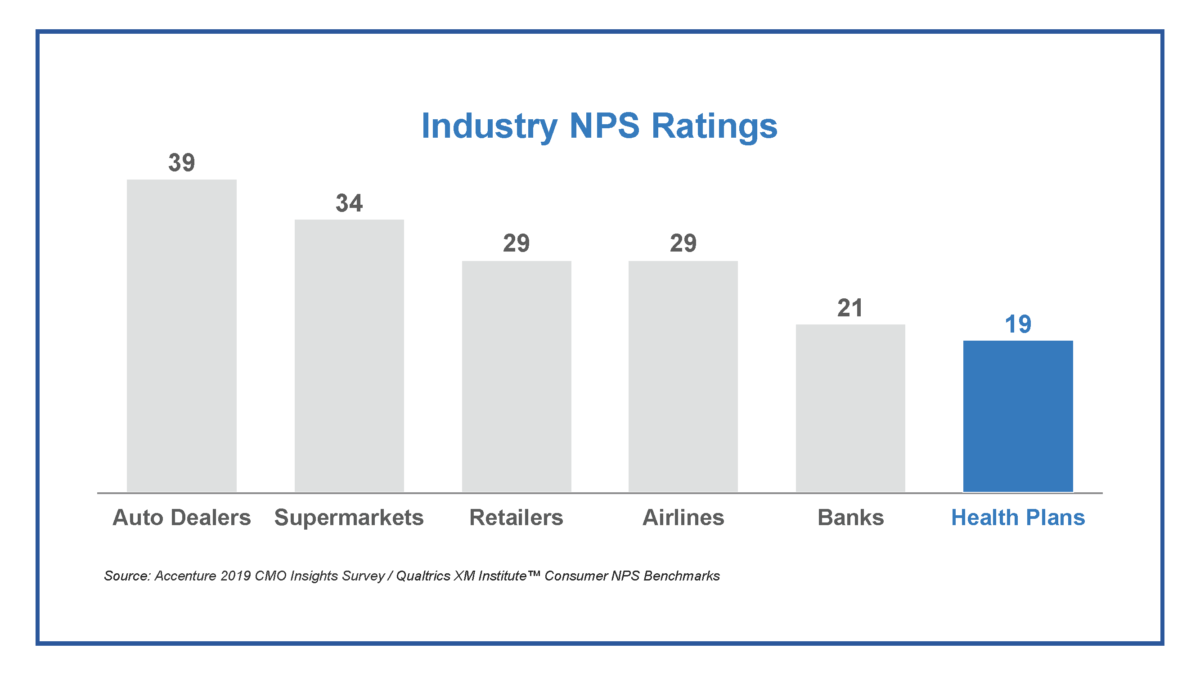
In a recent Accenture blog, the consultancy looked at how consumer experiences were ranked across industries. Health plans did not fare well. They ranked lowest in Net Promoter Scores (consumer experience ranking) behind auto dealers, airlines and banks — and far below payers’ own predictions for how they thought they would rank. With star ratings and QBPs expected to fall drastically in the coming year and member experience numbers (that accounted for one-third of star ratings in 2021) making up almost two-thirds by 2023, the need to prioritize how health plans engage and retain members is crucial.
So how do health plans approach building and maintaining more positive relationships with their members? At Wider Circle we believe there are substantial benefits to starting at the hyper-local level. This means truly investing in creating an authentic presence in the communities that they serve and cultivating meaningful relationships with the members within those communities. This also means finding innovative ways to enhance member engagement. There is no one-size-fits-all approach to fostering these connections especially when so many are not responsive to traditional remote engagement efforts. This is why offering a community-support network makes sense.
Our team is proud to be part of the solution for forward-thinking health plans. Since day one we’ve been focused on forming trusted groups of neighbors in a culturally-competent manner, with the goal of restoring the community support network critical for tackling the challenges in members’ lives and cultivating opportunities to motivate and support each other to get the care they need, when they need it, where they need it. Through peer-to-peer engagement rooted in trust, we have been able to implement “surprise and delight” programs that meet critical needs and enhance customer satisfaction to ensure positive ratings and retention, all at a lower healthcare cost.
As we enter 2022, health plans like Medicare Advantage are at a critical inflection point as they elevate their focus on improving key quality measures with an emphasis on enriching the consumer journey. By approaching this goal with an eye towards building trust and personalizing the experience to address individuals’ needs, we believe that plans will be well positioned to drive truly impactful change, ultimately helping their members to live happier, healthier lives.